
What is an EEG?
Table of Contents
Toggle“EEG” is the short-form of “Electro-Encephalo-Graphy”.
The literal translation is:
-Electro = Electrical
– Encephalo = head
– Graphy = Representation
Therefore, “Electro-Encephalo-Graphy” or EEG means “Graphs of the electrical activity inside your head”.

If my EEG is normal, does it mean that I do not have Epilepsy?
No. A normal EEG cannot guarantee that you do not have Epilepsy.
The diagnosis of Epilepsy is based on your clinical condition, rather than any one particular test. This is because there is no perfect test for Epilepsy.
A 1 hour EEG is normal in 50% of patients with generalized Epilepsy. Even more disappointingly, the EEG is normal in up to 70% of patients with focal Epilepsy.
A longer EEG (for example 4 hours) may show epileptiform abnormalities missed on a shorter EEG. Also, if you are sleep deprived, the chances of your brain having small sparks that can be seen on EEG increases. Therefore, many doctors will ask you to sleep for only 4 hours the night before the EEG. This is called a “Sleep-Deprived EEG”.

If my EEG is abnormal, does it mean that I have Epilepsy?
Usually, with two caveats.
First, rarely, a person who does not have Epilepsy may still have Epileptiform discharges on their EEG. We doctors don’t know what that means. Perhaps these people are at a slightly higher risk of seizures. However, this increase in risk, if at all present, is minimal. Treatment with anti-epileptics is not required unless the person is actually having seizures. Avoiding sleep deprivation, stress and excessive consumption of alcohol would be very reasonable.
Second, occasionally, normal waves on the EEG may be mistaken for epileptiform discharges. There are many normal waveforms (such as “Wickets”) which look sharp and may be mistaken for abnormal electrical sparks. A second review of the EEG may be helpful in such a scenario. Indeed many epilepsy experts will ask other experts about their opinion when they encounter a particularly odd-looking shape on the EEG.
Here is an excellent paper that describes Epilepsy genes causing channelopathy [Bartolini et al 2020].
What are “Epileptiform Abnormalities”?
As explained here, the different parts of our brain communicate with each other using electricity. Usually, this electricity is very strictly regulated. Occasionally, however, a small part of the brain may have an electrical storm.
This electrical storm produces abnormal bursts in electricity which can be detected by the EEG. These abnormal bursts can produce many different kinds of shapes on the EEG, including spikes, short buzzes, and so on. These abnormal shapes are called “Epileptiform Abnormalities”.
What “Epileptiform Abnormalities” does an EEG show?
The type of Epileptic Abnormalities seen on an EEG depend on the type of seizures that you have./’
I have described them below for you to understand your EEG report properly. It may be worthwhile to look up the abnormality noted in your EEG report and find it in the tables below.
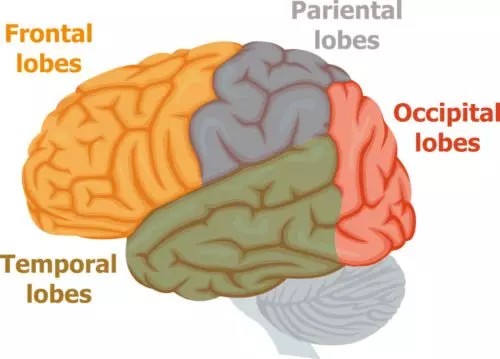
Depending on which part of the brain (see figure below) is producing these sparks, they are called Frontal, Central, Temporal, Parietal or Occipital. Sometimes, to indicate the exact location, a combination of these words is used. The exact location may identify your Epilepsy Syndrome. For example “Centro-Temporal” spikes are seen in an epilepsy syndrome called Rolandic Epilepsy.
If you have seizures that start in one part of your brain (Focal Seizures), then you usually get one of two epileptiform abnormalities:
Spikes/Sharps:
These are like a little electrical spark. The electrical spark produces a pointy wave on the EEG. If it is very pointy it is called a spike (<70 msec), whereas if it somewhat spread out it is called a sharp. Sometimes, a spike/sharp may be followed by a slow, gentle wave on the EEG, almost as if the brain was trying to quieten down the electrical storm. This particular sequence of events is called a “Local Spike-and-wave”
Fast activity: These are “buzzes” of abnormal electrical activity. They produce a hair-brush pattern on the EEG. Your EEG report will indicate the location as well, for example: “short episodes of temporal fast activity were seen”.

If you have buzzes on the EEG, it may indicate that you have Focal Cortical Dysplasia (FCD). FCD is described in more detail here.
If you have seizures that start all over the head at once (Primary Generalized Seizures), then you may get other kinds of epileptiform abnormalities on your EEG:
Generalized spike-and-wave:
The word “Generalized” means “all-over”.
These are similar to the spike-and-wave described above, except that these sparks happen all over the head.- They are sometimes seen more prominently in the front of the head, and sometimes it may be difficult to differentiate between a truly generalized spike-and-wave and a frontal spike-and-wave.- They may have multiple spikes in which case they are called “Polyspike-and-wave”. Polyspike-and-wave is seen in Juvenile Myoclonic Epilepsy (JME).- Your epilepsy syndrome determines the speed (technically, frequency) of these spike-and-wave discharges. For example:
| 3 Hz | Childhood Absence Epilepsy |
| Less than 3Hz | Lennox – Gastaut Syndrome (LGS) |
| More than 3 Hz | Juvenile Absence Epilepsy (JAE) or Juvenile Myoclonic Epilepsy (JME) |

Generalized Paroxysmal Fast Activity (GPFA):
These are similar to the fast activity described above, except it happens all over the head. Children with Lennox-Gastaut Syndrome (LGS)may have GPFA on their EEG.
However, all patients with GPFA do not have Lennox-Gastaut Syndrome – This is a common misconception, even amongst doctors. Even if your child has GPFA on his/her EEG, he/she may not have LGS. His/her entire clinical picture should be consistent with LGS. You can read more about LGS here.Electrodecremental pattern:
This pattern is relatively rare. An electro-decremental pattern is seen in Lennox-Gastaut Syndrome, during a particular type of seizure attack known as “Tonic seizures”, which can cause “drop attacks”. There is a sudden drop in brain activity on the EEG. This drop is usually short and lasts for 1-2 seconds. The child lurches forward during this time and may fall to the ground. These falls are also called “drop attacks”.
Continuous Spike-Wave in Sleep (CSWS):
This pattern is rare and is often missed. CSWS is like a near-continuous electrical storm inside the brain during sleep. The child seems to be sleeping peacefully.
CSWS is seen in children. This EEG pattern may be seen in conditions such as Landau-Kleffner, where children lose their power of speech.
It is critical, urgent and absolutely essential to record and overnight EEG in all children who lose their power of speech. Urgent treatment with steroids and other treatments prevent the marked damage to the brain produced by these electrical storms in sleep.
What other abnormalities can an EEG show?
Slowing:
If parts of your brain are working slowly, your EEG shows slow waves in that area. Again, your EEG report will state the location. For example: “Short episodes of frontal slowing were seen”.
Hypsarrythmia:
Hypsarrythmia is a rare EEG pattern. Hypsarrythmia is seen in a condition called “West Syndrome”, which is seen only in children. The EEG appears like a chaotic mess of slow waveforms. Unfortunately, hypsarrythmia on the EEG indicates that the entire brain’s function is severely disturbed.
Just like CSWS (see above), urgent and aggressive treatment decreases severe brain damage by this chaotic electrical activity.
Caution: This information is not a substitute for professional care. Do not change your medications/treatment without your doctor’s permission.
