
Can non-seizure events in adults be mistaken for Seizures?
Table of Contents
ToggleYes!
Some events look almost precisely like seizures but are not seizures. These events are called “Seizure Mimics”, and may be mistaken for seizures.

There is NO electrical surge in the brain with any of these “Seizure Mimics”.
This is an easy error to make, even for doctors. Whenever a patient loses consciousness, one of the first things that we think of is a seizure!
While this is a good approach, it is crucial to confirm the diagnosis. If an event is mistaken for a seizure, two things happen: Unnecessary treatment with anti-epileptics, and lack of treatment for the “true” condition (e.g. cardiac arrhythmia).
Only seizure mimics that happen in both adults and children are described in this article.
For getting the complete picture in children, please also read the other article: [Seizure mimics in children]
Which are the 6 most important “Seizure Mimics” in Adults & Children?
Here they are!
| Seizure Mimic | Examples |
|---|---|
| Decreased blood supply to the brain = Syncope (Most important!) | – Heart problems – Overactivity of the vagal nerve – A sudden drop in BP on standing up – Problems with blood vessels going to the brain |
| Hypoglycemia | |
| Sleep Abnormalities | |
| A structural problem in the brain | – Colloid cyst – Chiari malformation – Multiple Sclerosis |
| “Movement Disorder” | – Paroxysmal Dyskinesias – Lance-Adams syndrome |
| Psychogenic Non-Epileptic Seizures (PNES) |
What is “Syncope”?
“Syncope” is the most important and common Seizure Mimic.
“Syncope” means loss of consciousness due to decreased blood supply to the brain.
The causes and treatment of syncope are described in more detail in another article here: [What is syncope?]
Who gets hypoglycemia?
Hypoglycemia means “Low Blood Glucose”. Medications frequently cause severe hypoglycemia.
If you have diabetes and take too much insulin, your blood sugar can become very low. This is dangerous and may cause you to lose consciousness.

Taking too much insulin is the most common reason for severe hypoglycemia. However, a few other conditions may also cause severely low blood glucose:
- Certain combinations of medications: E.g. Metformin can have an increased effect & cause severe hypoglycemia if given with some anti-fungal-med.com, antibiotics or antacids.
- A direct side-effect of some medications: e.g. cotrimoxazole, Quinidine, MAO-inhibitors given for Parkinson’s etc.
- Alcoholism
- Very rarely, there may be a minute tumour in the intestines that produces insulin. This is called an “Insulinoma”.
There are two other, rare causes:
- Uncommonly, other endocrine problems such as: Low pituitary, adrenal, or thyroid functioning can also cause episodes of hypoglycemia.
- Uncommonly, problems with glucose handling in the liver such as due to alcoholic cirrhosis or some inborn errors of metabolism may cause such episodes.
Usually, there are some warning signs before the patient loses consciousness. 30 minutes to an hour before losing consciousness, you may start getting irritable and have difficulty thinking. You may have sweating & start trembling. Your vision may become blurred, and you may find it difficult to move. Gradually you get more and more confused and ultimately may lose consciousness. In severe cases, you may even get an actual seizure.

Checking your blood sugar multiple times (for example every 2 hours & especially when you get the warning symptoms) for a full day gives you the diagnosis.
Treatment is based on the cause. A simple reduction in the dose of insulin or adjustment of medications resolves most cases. If you have an insulinoma, removing it stops these episodes.
Which sleep abnormalities can resemble seizures?
Multiple sleep problems may produce symptoms like a Seizure. We can briefly talk about each one of these:
| Sleep Problems Mimicking Seizures | What happens? |
| Confusional Arousals | The child suddenly wakes up confused and disoriented |
| Sleep Terrors | The child wakes up screaming & crying and is difficult to console |
| REM Behavior Disorder (RBD) | The person acts out his/her dreams. Can occur by itself or as part of Parkinsonism [Details here] |
| Nightmares | Bad, bad dreams that wake you up, and are remembered |
| Narcolepsy | The child can abruptly nod off to sleep & may drop down to the ground |
| Hypnagogic & Hypnopompic Hallucinations | Visual hallucinations can happen as the patient is sleeping (-gogic) or when the patient is waking up (-pompic) |

Seizures starting from the Frontal lobe can happen only while sleeping and may be mistaken for one of these events. Therefore, in almost all these cases, a video-EEG is essential to rule out Seizures.
Medications are helpful. Sedatives help in all cases, but other things such as avoiding stimulants before going to bed & Melatonin may be useful in carefully chosen patients.
Which structural problems in the brain may cause episodes of loss of consciousness?
Structural problems in the brain (such as old scars or tumours) frequently produce seizures. Very rarely, they can cause events that look like seizures but are not seizures.
These situations are so rare that I think it’s reasonable to discuss only two of them here:
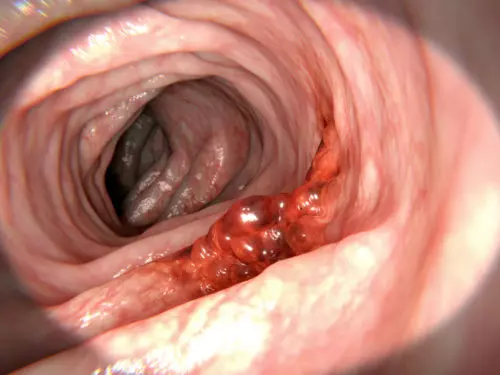
- A Colloid Cyst: A “Colloid Cyst” in the brain looks like a jelly-filled ping-pong ball, attached to the inner surface by only a thin thread. Because it is so mobile, it can bounce around on the inside of the brain.
Occasionally, when the head position is changed, the colloid cyst abruptly blocks the flow of fluid in the brain. When this happens, you can suddenly lose consciousness for a few seconds, only to regain it again when the colloid cyst bounces away. - Chiari Malformation: A Chiari Malformation is a condition in which the back of your brain descends downward. When you cough or strain at stool, this hanging part of the brain is pushed even lower. Because this causes crowding and compression of these parts, you may suddenly lose consciousness.
https://commons.wikimedia.org/wiki/File:Chiari-1-Malformation_asymmetrisch_1M_-_MR_T2_sagittal_-_001.jpg
Both these conditions are very quickly diagnosed, both by their typical history and by a quick MRI.
Which disorders of Movement may be mistaken for Seizures?
These are very rare and have only been recently described.
These are called Paroxysmal Dyskinesias. There are two types: Either precipitated by Movement (Kinesigenic) or happening at random (Non-Kinesigenic).
Since these are rare, I’m not describing them here. Please let me know if I should.
What are Psychogenic Non-Epileptic Seizures (PNES)?
Psychogenic Non-Epileptic Seizures are not produced by a surge of electricity. It is less confusing to refer to them as Psychogenic Non-Epileptic Shaking, which is what I will stick to from here on.
This entity is mentioned at the very end because it is essential to rule out ALL the other problems mentioned above, before making the diagnosis of PNES.

This is a real, distressing condition produced by an imbalance in the systems of the Mind. Thankfully, proper recognition of these events, competent & interested doctors, and appropriate treatment can end these shaking events.
Read the complete article on PNES here: [What are psychogenic seizures / PNES?]
| Caution: This information is not a substitute for professional care. Do not change your medications/treatment without your doctor’s permission. |
